Medical Emergencies NCLEX-RN
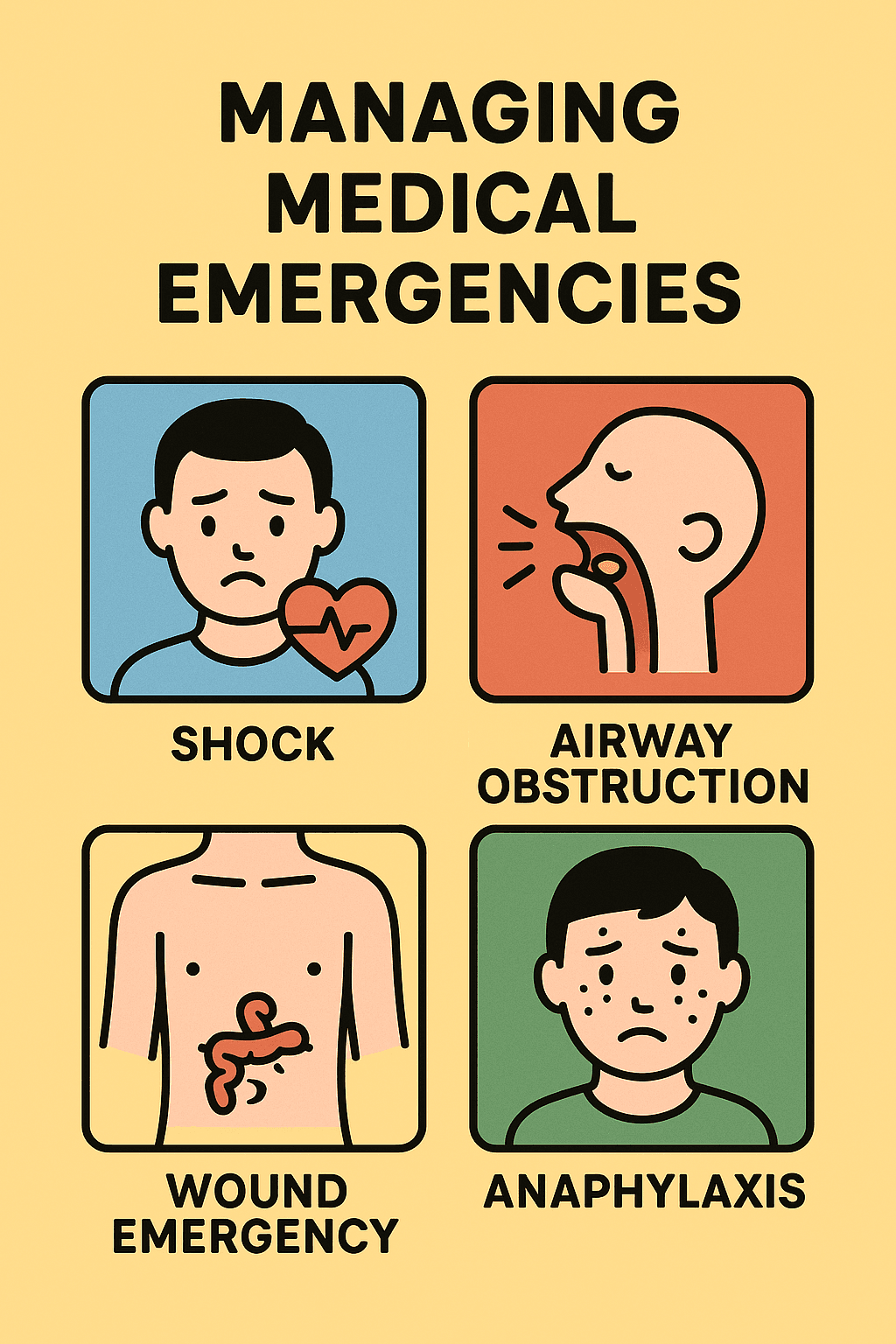
Clinical reasoning in acute situations such as shock, airway compromise, wound emergencies, anaphylaxis, cardiac arrest, and neurological crises
~7 min read
🎓 Listen to Professor Narration
Too lazy to read? Let our AI professor teach you this topic in a conversational, engaging style.
Overview
Welcome, future nurses! In this session, we’ll break down key concepts essential for managing medical emergencies as highlighted in recent NCLEX-RN style scenarios. By the end, you’ll be equipped to recognize critical signs, understand priority interventions, and confidently apply clinical reasoning in acute situations such as shock, airway compromise, wound emergencies, anaphylaxis, cardiac arrest, and neurological crises. Let’s dive into the practical “why” and “how” behind emergency nursing care—so you’re ready to act fast and save lives.
Concept-by-Concept Deep Dive
Recognition and Initial Management of Shock States
What it is:
Shock is a life-threatening condition where tissue perfusion is inadequate to meet cellular needs. This can be hypovolemic, distributive (e.g., septic, anaphylactic, neurogenic), or cardiogenic in origin.
Types and Features
- Septic/Toxic Shock: Often triggered by infection (e.g., toxic shock syndrome), leading to vasodilation, hypotension, fever, and sometimes rash.
- Anaphylactic Shock: Rapid allergic response with airway edema, hypotension, and urticaria.
- Cardiogenic Shock: Resulting from cardiac pump failure, such as after myocardial infarction.
Step-by-Step Nursing Actions
- Early Recognition: Monitor for hypotension, tachycardia, altered mentation, and skin changes.
- Immediate Interventions: Ensure airway and breathing, supply oxygen as needed, establish IV access, and anticipate fluid resuscitation or medication administration per protocol.
- Monitoring: Continuous vital sign monitoring, assess for urine output, and watch for progression to multi-organ dysfunction.
Common Misconceptions
- Mistaking fever alone as benign: Always consider the context—fever with hypotension and rash is a red flag.
- Delaying intervention until labs return: In emergencies, act based on clinical suspicion while awaiting confirmation.
Airway Emergencies and Obstruction
What it is:
Any event compromising the airway—due to allergic reactions, swelling, foreign bodies, or injury—demands rapid identification and response to preserve oxygenation.
Key Components
- Tracheostomy Care: Includes assessment of airway patency, tube placement, and monitoring for obstruction or dislodgement.
- Choking and Obstruction: Recognize the difference between complete and partial airway blockages.
Step-by-Step Reasoning
- Assessment: Look for stridor, use of accessory muscles, inability to speak/cough, or cyanosis.
- Immediate Action: For total obstruction, perform abdominal thrusts (if appropriate) or back blows in infants. For partial obstruction, encourage effective coughing if present.
- Post-Intervention Monitoring: After resolving an obstruction or placing a tracheostomy, closely monitor for hypoxia or re-obstruction.
Common Misconceptions
- Assuming all airway emergencies require immediate intubation: Sometimes less invasive measures are indicated first.
- Neglecting reassessment post-intervention: Airway can re-occlude or complications may arise.
Wound Dehiscence and Evisceration
What it is:
These are surgical complications where wound layers separate (dehiscence), or internal organs protrude through the wound (evisceration).
Components
- Recognition: Sudden "popping" sensation, visible separation, or protruding viscera.
- Priority Actions: Protect the exposed organs and prevent further injury or infection.
Action Plan
- Stay with Patient: Call for help immediately.
- Cover Wound: Use sterile, saline-moistened gauze to cover exposed organs without applying pressure.
- Positioning: Place client in low Fowler’s position with knees slightly flexed to reduce abdominal tension.
- Do NOT: Attempt to reinsert organs or leave the wound exposed.
Misconceptions
- Applying dry dressings: Can cause tissue dehydration and more injury.
- Forgetting to bend knees: Increases tension on wound edges.
Cardiac and Respiratory Arrest: Immediate Nursing Response
What it is:
Sudden cessation of effective cardiac output or respiration requires rapid, coordinated intervention to prevent death and neurological injury.
Key Steps
- Unresponsiveness: Always check for responsiveness and pulse before proceeding.
- CPR and Defibrillation: High-quality chest compressions and, if indicated, defibrillation are priorities.
- Advanced Airway Management: Ensure adequate ventilation and oxygenation.
Stepwise Reasoning
- Assess: Tap/shout and check pulse.
- Call for Help: Activate emergency response or code blue.
- Start Chest Compressions: If no pulse, begin CPR immediately.
🔒 Continue Reading with Premium
Unlock the full vlog content, professor narration, and all additional sections with a one-time premium upgrade.
One-time payment • Lifetime access • Support development
Join us to receive notifications about our new vlogs/quizzes by subscribing here!